Take it from me, there’s not a fat person alive in this country, from infant to ancient, who hasn’t been told they should lose weight to be healthy.
This is a lie.
Numerous medical studies have found many overweight people have some life-threatening illness, and obesity can in some cases exacerbate the symptoms of that illness. However, there are two important points these studies have, until recently, failed to consider: correlation is not causation, and many thinner people also suffer these same illnesses.
No disease has been proven to be a symptom solely of being fat. Even in Type II Diabetes, about 20 percent of sufferers are normal weight according to the National Institute of Health. In many cases, it’s likely obesity is actually a symptom of a disease.
Recent studies show fatness has nothing to do with fitness. In 2013, Dr. Vaughn Barry, Ph.D., collected and analyzed the data of 10 studies on the mortality rates of people judged to be cardiovascularly fit or unfit, relative to their body mass index. Barry found those who were unfit had twice the mortality rate of those who were fit, regardless of BMI.
In other words, it’s just as unhealthy to be thin and weak as to be fat and weak, and it’s just as healthy to be fat and strong as to be thin and strong.
Losing weight and keeping it off is not as simple as the weight loss industry wants us to believe. Dr. Tracy Mann, professor and researcher at University of Minnesota, said diets don’t work long term. “You don’t just notice [food] — it actually begins to look more appetizing and tempting,” Mann said in an interview for the Washington Post last year. “So the thing you’re trying to resist becomes harder to resist.”
In 2001 I tried the Atkins diet for about a month. The pounds melted off. My jeans went from lay-down-to-zip to literally falling off my hips. I was ecstatic – and I was miserable. I couldn’t stop thinking about food. I counted carbs obsessively, even when I wasn’t hungry, planning for my next meal. At parties I couldn’t eat anything: all the food was sugar- and flour-laden. The day I caught myself standing with my head in the pantry smelling that precious loaf of bread with just 10 carbs per slice – I could have a whole sandwich! – I realized I had a food obsession, one I never had before I tried to lose weight.
Bariatric surgery is no better. It may reduce the amount of food one can eat at once, but this can result in constant eating. At the same time, some types of surgery can starve the body of crucial nutrients, regardless of the food eaten, because it bypasses parts of the digestive system that absorb those nutrients.
Furthermore, the body reacts to what it perceives as starvation by holding on harder to every calorie it gets. “Your body uses calories in the most efficient way possible,” Mann said, “which sounds like a good thing, and would be good thing if you’re starving to death. When your body finds a way to run itself on fewer calories, there tends to be more leftover, and those get stored as fat, which is exactly what you don’t want to happen.” Before long, many patients are just as fat as they were before, if not fatter.
However well meaning, “encouraging” fat people to lose weight is not only unhelpful, it’s actively detrimental. In a 2013 study, Angelina Sutin, psychologist and assistant professor at Florida State University College of Medicine, showed weight discrimination is more likely to result in targets of discrimination gaining more weight than losing it.
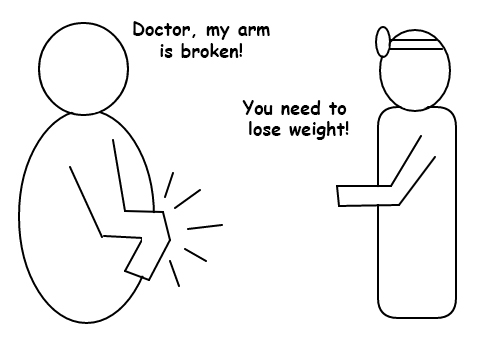
The worst offenders are doctors with fat-prejudice. Doctors say a thing is so and everyone believes them; they went to school for eight years or more, they must know what they’re doing. But doctors are only as good as the most recent studies they have read, and many don’t seem to continue learning once they have their degrees. Worse, some do read new information, but decide it’s wrong because it refutes what they believe.
Many doctors see a fat patient and make the snap diagnosis of obesity, regardless of the actual problem. The blog “First, Do No Harm” at fathealth.wordpress.com, has hosted people’s stories of belittlement, misdiagnosis and outright mistreatment of fat patients since 2007, and the stories keep coming.
Size discrimination is the last socially acceptable bigotry, and it needs to stop. What’s good for one body is not good for every body. Pretending one size fits all hurts people and helps no one.